Pregnancy
Cesarean Delivery


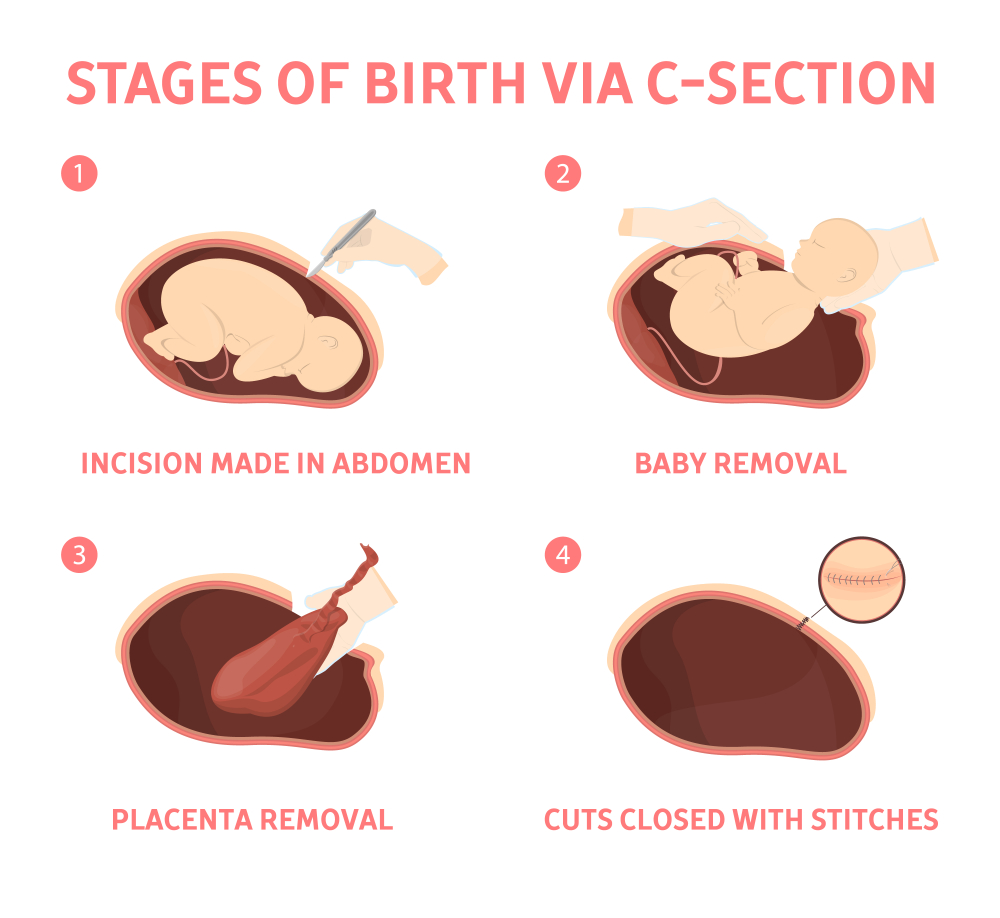
If you’re pregnant, knowing what to expect during a C-section — both during the procedure and afterward — can help you prepare better.


Why It's Done
Sometimes a C-section is safer for you or your baby than is a vaginal delivery. Your health care provider might recommend a C-section if :
- Your labor isn’t progressing : Stalled labor is one of the most common reasons for a C-section. Stalled labor might occur if your cervix isn’t opening enough despite strong contractions over several hours.
- Your baby is in distress : If your health care provider is concerned about changes in your baby’s heartbeat, a C-section might be the best option.
- Your baby or babies are in an abnormal position : A C-section might be the safest way to deliver the baby if his or her feet or buttocks enter the birth canal first (breech) or the baby is positioned side or shoulder first (transverse).
- You’re carrying multiples : A C-section might be needed if you’re carrying twins and the leading baby is in an abnormal position or if you have triplets or more babies.
- There’s a problem with your placenta : If the placenta covers the opening of your cervix (placenta previa), a C-section is recommended for delivery.
- Prolapsed umbilical cord : A C-section might be recommended if a loop of umbilical cord slips through your cervix ahead of your baby.
- You have a health concern : A C-section might be recommended if you have a severe health problem, such as a heart or brain condition. A C-section is also recommended if you have an active genital herpes infection at the time of labor.
- Mechanical obstruction : You might need a C-section if you have a large fibroid obstructing the birth canal, a severely displaced pelvic fracture or your baby has a condition that can cause the head to be unusually large (severe hydrocephalus).
- You’ve had a previous C-section : Depending on the type of uterine incision and other factors, it’s often possible to attempt a normal delivery. In some cases, however, your health care provider might recommend a repeat C-section.
OR
- Labor is not progressing.
- Multiple pregnancy, such as twins or triplets, have occurred.
- The fetus experiences an emergency or severe health concern.
- The fetus has excess fluid on the brain.
- The fetus is in the breech or transverse position.
- The baby is too large to travel through the cervix.
- The mother has a contagious virus, such as herpes or HIV, that a vaginal birth would transmit to the infant.
- The mother has complicating conditions, such as diabetes or high blood pressure.
- The mother has a uterine condition or a fibroid obstructing the cervix.
- The placental or umbilical cord has anomalies.
- The mother has previously given birth via C-section.
Risks
- Potential problems the mother can experience include :
- wound infection
- blood loss
- blood clots
- injury to an organ, such as the bowel or bladder
- adverse reactions to medication or anesthesia
- potential complications during future pregnancies
- Some women may also experience endometritis, an infection of the lining of the uterus.
Infants Risk
- Surgical injury and breathing difficulties, or respiratory distress syndrome.
Recovery After C-Section
Following a C-section, you and your baby can expect to remain in the hospital for 2–4 days.
While you recover, the following things may happen:
- Mild cramping, especially if you are breastfeeding
- Bleeding or discharge for about 4–6 weeks
- Bleeding with clots and cramps
- Pain in the incision
- You have to make a note that the severity of these symptoms and recovery varies from women to women different
- Your doctor will recommend you for restricting physical activity on returning home and resuming normal activity is safe, typically 4–6 weeks after surgery,
- Your doctor will recommend you to avoid strenuous exercise, lifting heavy objects, placing anything in the vagina, or having sex.
During the recovery period, a woman can take the following steps:
- maintain hydration by drinking plenty of water
- take any medications as directed
- rest when necessary
- provide support to the incision and abdomen with the use of a pregnancy belt or pillow
Pregnancy Do’s and Don’t That May Surprise you!
Pregnancy Do’s
- Do Get Your Screenings
- Get screened to assess a baby’s Down Syndrome DS risk or other chromosomal abnormality even if you are below age 35.
- Do Gain Weight the Smart Way
- Packing on the pounds causes health complications Gaining too much in pregnancy sets you and your baby up for weight problems later on in life and put you at greater risk for gestational diabetes and hypertension
- Below, find out how much weight you should put on:If your are,
- Underweight : Gain 28 to 40 pounds.
- Normal : Gain 25 to 35 pounds.
- Overweight : Gain 15 to 25 pounds.
- Obese : Gain no more than 20 pounds.
- Do Visit Your Dentist
- Do Visit Your Dentist
- Routine dental care helps to prevent serious issues like preterm labor.
- Skip cosmetic procedures, such as whitening, but get regular checkups. Have your teeth cleaned at least once during pregnancy.
-
- Fluctuating hormone levels can cause expecting moms to develop swollen, bleeding gums
- Left untreated, it can lead to periodontal disease, which raises your risk for low weight and premature delivery sevenfold
- Do take prenatal vitamins
- Take prenatal vitamins and supplements recommended by your healthcare provider.
- Eat a healthy diet
- Learn about good nutrition for you and for your new family
- Do drink plenty of water
- Drink plenty of water. You can have approximately 1.5 liters (about 6-7 cups, or 3 water bottles) of water daily.
- Do have sex
- Continue making love if it is comfortable.
- Sex during pregnancy is fine, as long as you don’t have a complicating factor such as placenta previa or another type of high-risk pregnancy.
- Do Get sleep:
- Rest more! Sleep an extra hour every night. Try to alternate activities with breaks. Aim for 7-9 hours of sleep each night.
- Changing hormone levels, anticipation, and anxiety can make deprive sleep during your 9 months of pregnancy,especially in the final trimester, you’ll need your sleep.
- Take a quick snooze if you feel tired and schedule naps whenever you can. Set bedtimes and stick to them.
- Do schedule a flu shot
- Get a flu vaccine as long as you don’t have a contraindication
- It will protect you as well as your developing fetus.
Pregnancy Dont’s
- DO Not drink alcohol
- Alcohol use during pregnancy is the primary known cause of developmental disabilities and birth defects
- Stop Smoking
- Smoking during pregnancy exposes your baby to toxic, cancer-causing chemicals and decreases the amount of oxygen and nutrients for your baby.
- Smoking and exposure to secondhand smoke can lead to miscarriage, high blood pressure, low birth weight, asthma, colic, childhood obesity and increased risk of sudden infant death syndrome
- Avoid Hot Tubes
- They can raise your body temperature which may disrupt fetal development. Weekly hot tub sessions double the risk for miscarriage
- Skip Raw, Unpasteurized, or Processed Foods
- Raw fish, Hot dogs, deli meats, and unpasteurized juices and dairy products may contain Listeria bacteria, which can be fatal for your fetus. However, pasteurized juices and dairy items are safe.
- Don’t drink a lot of caffeine
- Caffeine can travel through the placenta and increase your baby’s heart rate.
- You can safely consume a cup or two of coffee/tea each day, but forego downing a triple-shot latte while you’re carrying.
- Don’t self medicate yourself
- Avoid medications including herbal supplements and over-the-counter medications unless prescribed by your doctor.
- Avoid toxic fumes and chemicals.
- Stay away from chemicals like insecticides, solvents, LEAD, mercury, and paint.
- Many of these items can be found in household cleaners and paint and not all have warnings on their labels
- Additionally, DON’T clean the litter box. You could put yourself at risk for toxoplasmosis, an infection that is very harmful to the fetus.
Working Out for Two
During pregnancy the question of whether to continue or begin an exercise program to optimize health for both mom and baby often arises.
The first step to help answer this question is a visit to your doctor.
While exercise during pregnancy is usually encouraged, under some circumstances exercise can be detrimental to both the expecting mother and the growing fetus. Only after a thorough clinical evaluation can a physician determine your exercise risks, if any.

1. How the Body Changes During Pregnancy
- It’s no secret that your chest and abdomen grow as your baby gets bigger. But there are other underlying changes that take place, all of which can affect your ability to exercise the way you may be used to. Here are a few.
2. Guidelines for Exercise during Pregnancy
- Despite these changes, exercise during pregnancy can be safe for you and baby.
- Not only does it helps to maintain fitness, but it can improve the body’s ability to cope with labor, delivery, and recovery.
- The ACOG recommends at least 30-60 minutes of physical activity on most days of the week to reap these benefits.3
- https://www.acog.org/Patients/FAQs/Cesarean-Birth?IsMobileSet=false;Adapted from The American College of Obstetrician and Gynecologists,cited on 9th Sep 2019
- https://www.rcog.org.uk/globalassets/documents/patients/patient-information-leaflets/pregnancy/pi-choosing-to-have-a-c-section.pdf, Adapted from Royal college of Obstetrician and Gynecologists, cited on 9th Sep 2019
- http://www.acog.org/Resources-And-Publications/Committee-Opinions/Committee-on-Obstetric-Practice/Weight-Gain-During-Pregnancy
- https://opentextbc.ca/anatomyandphysiology/chapter/28-4-maternal-changes-during-pregnancy-labor-and-birth/;cited on 4th Sep 2019.
- Vincenzo berghella MDa , Gabriele Saccone MDb, April 2017 Volume 216, Issue 4, Pages 335–337; Exercise in pregnancy!;Adapted from https://www.ajog.org/article/S0002-9378(17)30130-8/fulltext